Cauda Equina Syndrome
It is a scary thought to have burning numb pain in the groin area coupled with lower limb weakness and reduced bladder and bowel control. However, this disease does exist, and it is called Cauda Equina syndrome. Follow along this blog to see what this issue entails and what can be done about it!
What is it?
Cauda Equina syndrome (CES) is a neurological condition where the lower tail end of the spinal cord is compromised (often compressed). Cauda equina meaning horse’s tail in latin pertains to the spinal nerve pairs coming from lumbar sacral and coccygeal nerves. Although CES is a rare condition, 45% of all cases precipitate following a large lower lumber disc herniation, prolapse or sequestration. CES may also be caused by smaller prolapses in the presence of spinal stenosis. Other triggers may involve epidural hematoma, infections, neoplasms, ankylosing spondylitis and even trauma. It is a very rare condition comprising around 2–6% of lumbar disc operations. Its incidence varies between 1 in 33,000 to 1 in 100,000.
Hallmark red flag symptoms of Cauda Equina syndrome include:
- Severe low back pain
- Bilateral sciatica – especially at a L5/S1 distribution
- Saddle and genital sensory disturbances
- Bladder, bowel and sexual dysfunction
Onset of symptoms may vary between hours to months. Depending on the extent of the syndrome, it may also be defined as incomplete or complete. When the syndrome is incomplete, patients may only have altered urinary sensation, loss of urgency/desire to void and the need to strain when micturating. Saddle and genital sensory deficit is often unilateral or partial and trigone sensation should be present. If there is a complete syndrome, the characteristics is still painless urinary retention and overflow incontinence. This is couples with significant saddle and genital sensory loss.
Contingent on the type of CES, different management strategies may be appropriately prescribed. The general consensus is to urgently seek a concrete diagnosis of your symptoms, then opt for surgical treatment for severe, complete cases or continue careful monitoring for modest incomplete cases. All cases are different as there are various stages of CES severity: CES suspected, CES incomplete, CES retention (where there is painless urinary retention) and CES complete. At the end surgery should be carried out as soon as possible for patient morale and comfort and because any delay in treatment can only worsen neurological recovery with the possibility of continuing damage to the more robust adjacent sciatic nerve roots which were previously uncompromised. The patient will most likely require urgent surgical decompression. Moreover timing of surgery is somewhat controversial and will be decided upon clinical and radiological review by the spinal surgeon.
Management protocol:
- Albeit a rare condition, CEW needs to be immediately treated, to avoid further clinical damage
- Early diagnosis by the GP allows them to check for urinary dysfunction, groin paresthesia, loss genital tone and neural deficits of the lower limbs
- Urgent MRI scan is the investigation of choice. Where this is unavailable a CT scan should be performed
- As a physiotherapist, our point of contact is less urgent to that of a GP, however on the rare occasion if it is a true case, we would immediately lease with the GP and also supportive multidisciplinary – potentially spinal surgeons, a urologist, a gynaecologist and other appropriate specialists.
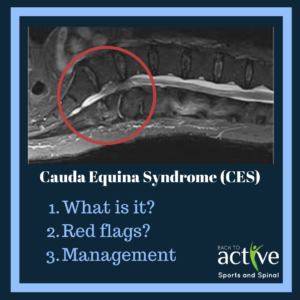
 Large central lumbar disc herniation at L4/5 and L5/S1 levels – warranting spinal decompressive surgery.
Large central lumbar disc herniation at L4/5 and L5/S1 levels – warranting spinal decompressive surgery.
Written by Joshua Shum Physiotherapist
