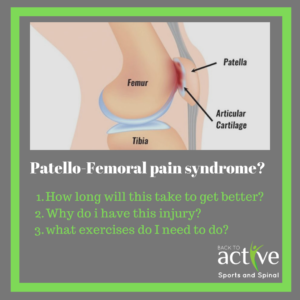
Knee cap pain (Patellofemoral pain syndrome)
It’s fun to play a nice hard game of soccer. Everything’s all fine and dandy, scoring a few goals here and there; and getting in that weekly exercise that doubles up as a social event. Except you’re starting to feel a ‘niggle’ (mild irritation) around your knee cap. You continue playing and this niggle then increases to an unbearable pain. This is Patellofemoral pain syndrome.
Questions to answer:
- How long will this take to get better?
- How will I get better/ what do I need to do specifically to get better?
- Will I get better?
- This injury came on after my knee surgery, is this normal?
What is it?
Patellofemoral pain syndrome is a complicated assortment of muscular imbalance. As there are number of different muscles acting on the hips and the knee cap, different tightness and weaknesses will cause the knee cap (patellar) to pull on an angle (patellar deviation). Since we heavily rely on our knees, whether it be crouching, walking, running, hopping and jumping, that constant discomfort in our knees due to poor patellar tracking will progressively get worse. This is because we are introducing wear and tear to the underside of our knee cap. What needs to be corrected here is the muscles imbalance, which will rectify the angle at which the knee cap pulls, ultimately eliminating pain.
The muscles involved in Patellofemoral pain syndrome include:
– Quadriceps
– Medial quadriceps/ vastus medialis oblique (VMO – the tear drop muscle)
– Iliotibial band (ITB)
– Hamstrings
– Glute medius
– Calf muscles
Even if one of these muscles is slightly stronger than the others it creates a disproportion and increases the risk of having Patellofemoral pain syndrome. However since this is largely an injury or muscular origin, we can almost guarantee that with the right exercise we may reset how our patella tracks. This injury is also common post ACL or meniscus injury. As we’re injured for a prolonged duration of time, we tend to lose bulk in that particular knee or we gain too much bulk in our uninjured leg – both of which may increase risk of developing patellofemoral pain syndrome. Therefore if we have had any reconstruction exercises, although it is common to develop this injury, we must be extra vigilant and proactive about rehabilitation.
It is also important to recognise that pure rest will not lead to recovery because the underlying cause of patellofemoral pain is the imbalance in our muscles. Rest may lead to symptom relief, however will not help us recover perfectly. Prognosis for this injury may take anywhere between 3 to 12 months for a full recovery.
Signs and Symptoms
– Pain when ascending/descending stairs, sitting with knees bent, kneeling, and squatting.
– Compressive forces directly on the knee cap
– Poorly localised pain around the knee area.
Risk factors
Risk factors are also characteristics that are screened for. Essentially risk factors are developed habits or attributes that make you more susceptible to the injury. If you have one of these risk factors, it does not guarantee that you will have this problem, however it indicates to us that you are at a higher risk of contracting this mechanical injury. Common risk factors include:
– Manual intensive occupation
– Age
– Gender
– Specific sports which are heavy on change of direction (netball, soccer, basketball, etc)
– Quadriceps and adductor strength
– Overweight (BMI >25)
Solution
Patellofemoral pain syndrome is often a difficult injury to treat as it involves isolating and pinpointing exactly which muscle is weak and which muscle is overpowering. Once diagnosed, clinicians may continue to prescribe you exercises to optimise biokinematics and the correct firing of particular muscles in a way that does no elicit pain. By continuing to perform exercises, this will help you get back into the sports and activities you want to do without any hinderance. Dry needling and taping will also help with this injury in its early stages.
In the early stages of patellofemoral pain syndrome, it is important to rest and ice. If pain is >5/10 when playing sport (volleyball, basketball, rugby, oztag, frisbee or any dynamic multidirectional sport as such) then avoiding playing is advisable until pain is kept < 3/10 consistently.
To substitute sport or your previous exercise routine, the following exercises will be beneficial for you:
introductory exercise (basic strength exercises for our VMO)
- Bridging with VMO bias (performing a bridge with a foam roller in between your legs – squeeze your legs together) 3 x 10
- Terminal knee extension with theraband 5 x 10
- Mini wall squats with VMO bias ((perform with a foam roller in between your legs – squeeze your legs together) 3 x 10
- Straight leg raise 3 x 10
- Ice twice daily over the kneecap (15 mins at a time)
Moderate exercises (VMO strengthening + balance component)
- Full wall squats with VMO bias
- Theraband clams
- Bosu ball squats
- Straight line lunges (+ harder variations of lunges)
- Single leg deadlift / romanian deadlift
- Cutting and running
- Barbell squats and deadlifts
Advanced exercises (balance + plyometric/sport specific)
- Sport specific tailored exercises
- Single leg squat (on bosu ball)
- Bound jumps
- Depth jumps
- Skater jumps (+ variations of skater jump)
- Running drills (for change of pace and change of direction)
Patellofemoral pain syndrome may be treated through exercise and it is preferable that professional advice is sought before the injury progresses to extreme conditions. By getting on top of this problem, professional physiotherapy may also help you run faster, jump higher and achieve overall sport specific improvements.
Written by Joshua Shum Physiotherapist
