Mallet Finger 
Mallet finger is a very uncommon injury, often coined as baseball finger to describe the unexpected striking of a baseball onto the tip of the finger; forcing it to bend further than it is intended to go. This injury is not exclusive to baseball but may occur in other high velocity ball sports where there is a chance of catching a ball at high impact (volleyball, basketball, rugby, etc). Mallet fingers are most commonly found in men, specifically the middle finger on the dominant hand.
What is it?
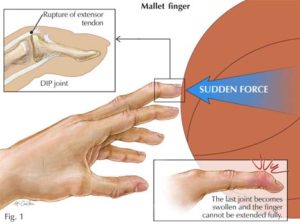
Mallet Finger is a passive flexion deformity due to the rupturing or avulsion (pulling away from bone) of the extensor mechanism on our finger. Think about our finger having two sets of wires. The ones on the front pull our fingers into a fist under the pad of each fingertip while the wire underneath our fingernails open up our fingers again. If the wire on the backside of our finger is compromised (most commonly at the last digit of our fingers) then our finger will passively be oriented in a flexed position.
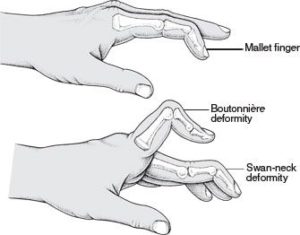
At the start patients may choose to ignore this deformity. However, in the long run of this, deformations may increase to a swan neck deformity. This is the bowing of the digit preceding the distal finger joint. As the finger bends into flexion at the end, the penultimate joint bows into extension.
Signs and Symptoms
Common signs and symptoms amongst acute cases of mallet finger is bruising along the DIP joint, that is the last joint of every finger. However, even then bruising, swelling and tenderness don’t often occur.
All mallet finger cases will also fail to fully extend their finger. Yet this continues to not be an issue due to the lack of activities that require full finger extension. Therefore, the patient’s perception of the severity of this issue is reduced. When seeking a therapist, if the therapist is able to successfully passively move your finger into full extension, it is indicative that a mallet finger is present.
Solution?
Fortunately, not all cases of mallet finger requires surgery. Closed mallet finger injuries are treated with an immobilisation splint in extension for 8 weeks. If the splint is ever removed then full immobilisation is required again. Splinting can be started even as late as 3 months post injury. Once the splint is used, occasional splinting may be used to avoid high risk activities (manual labour, sports and during sleep – Yes we roll around when we sleep!). Post splinting, physical clinicians may aid in offering tapered exercises back to full strength functionality. This includes performing basic range of motion and isometric exercises first before coming back to quick dynamic exercises.
Written by Joshua Shum Physiotherapist
