Shin Splints/Medial tibial stress syndrome (MTSS)
Here’s a question for the more recreational runners and avid trainers, have you heard or ever suffered from shin splints? In one leg? In both legs? If you’ve ever had it you’ll know that the pain is unbearable and throws a rather cumbersome spanner in the works. It is athletically debilitating and also takes a frustratingly long time to remedy. In truth Medial tibial stress syndrome (MTSS) is multi-factorial and involves training errors and various biomechanical abnormalities.

What is it?
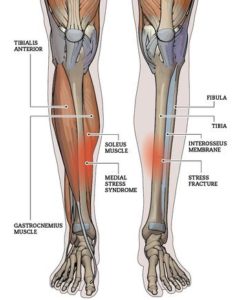
In short MTSS is a stress fracture caused by repetitive loading stress during running and jumping. As a result, bony resorption outpaces bone formation of the tibial corex. However recent evidence tells us that MTSS is beyond just a simple bruising of the bone and a fracture however it is all 4:
- Tendinopathy of adjacent muscles (shin and back of shin musculature – tibialis posterior, tibialis anterior, and soleus muscles are also commonly implicated)
- Periostitis – inflammation of band of tissue that lies on top of bone
- Periosteal remodelling – ongoing maintenance of that same band of tissue
- Stress reaction of the tibia.
The incidence among physically active soldiers is 7.9%, and among athletes it varies between 4% and 35%. Runners who frequently do long distance running or greater than 32 km’s a week have a high chance of contracting this injury too. However, this magnitude of training is not exclusive to runners but also found in other ballistic sports, such as football, basketball, soccer, and dancing. Therefore, MTSS is also found in these sports that involved high explosive movements.
So how does MTSS actually feel?
The most common complaints of patients with MTSS will sound vague, the onset of pain is also poorly noticed as it is a conglomerate of a few issues (some which will occur asymptomatic until a certain tipping point). There will be vague diffuse pain in generally, sharp pain along the inside or outside ridge of our shin bone after exercise and sharp pain along the same ridges when massaged or palpated (the pain is easily localised when pressed and occurs on the middle to distal end of the tibia (shin bone). If there is pain along a length greater than 5cm along the tibia then, it is a true case.
Risk factors that will increase MTSS:
- Longstanding smoking and stamina deficits
- Flattening of the longitudinal arch of the foot
- Poor hip mechanics and rotation
- Obesity
- Poor running biomechanics
- High exposure to uneven terrain while training
- Running on hard surfaces
- Poor training structure – overloading, avoiding rest, running too fast for their own good.
- Women have an increased susceptibility for this issue potentially due to hormonal differences and imbalances.
So how is MTSS solved?
The crux of treatment lies in resting and icing. This is crucial for any acute inflammatory response. However, prolonged rest from activity is not ideal, and other therapies are necessary to help the athlete return to activity quickly and safely. Retraining proper biomechanics for running, knee orientation, ankle orientation, improving hip stability and foot arch stability create a shotgun approach towards getting over MTSS – the patient will need to understand that re-learning all these facets will take a long time, but will also inevitably be a worthwhile investment in reducing reinjury. Within the acute phase use of local NSAIDS (voltaren rub and other topicals) will be very beneficial too.
During the subacute stage, while re-learning biomechanics, the athlete will have a tapered approach towards running and sport. He or she may continue running, however at a significantly decreased length and pace (at least 50% or more for running distance, frequency and intensity). Stretching and strength drills will be implemented and other physical activity adjuncts such as taping and dry needling may also be considered. Athletes will immensely benefit from low impact activities such as: pool running, swimming, elliptical machine, or riding a stationary bicycle

Ideally these are the summary of treatment goals for MTSS:
- Rest and ice in the acute phase
- Modify training program: decrease intensity, frequency, and duration
- Use low-impact and cross-training exercises during rehabilitation period
- Gradually return to sport with pain-free activity
- Perform regular stretching and strengthening exercises
- Wear proper-fitting shoes with good shock absorption
- Consider orthotics if indicated
- Female athletes may have special considerations
- Treat key biokinetic dysfunctions
Finally, medical scans and surgery is only recommended if conservative training fails. There is a probation period of at least 12 – 20 weeks of conservative treatment.
All MTSS cases are painfully annoying to isolate a specific cause. This is because it is a multifaceted injury. MTSS or shin splint clients should seek professional help immediately before the issue progresses and continues to degenerate. These issues are amenable through specific core/ balance, low impact and strength exercises; whilst also implementing a graded approach back to sport
Written by Joshua Shum Physiotherapist
