What is temporomandibular disorder (TMD)?
A temporomandibular disorder (TMD) is a prominent injury affecting up to 33% of the population. TMD is often viewed as a repetitive stress injury of the masticatory/chewing muscles and structures; and has many similarities to musculoskeletal disorders of other parts of the body. TMD is generally treated by a combination of physiotherapists, dentists and clinical psychologists as this particular injury is very complex and affected by all ortho-, musculo- and psychological factors.
How does TMD feel?
TMD pain is often described as a poorly localised jaw pain that often radiates to the same side of the face. This is because jaw and face (orofacial pain) is innervated and distributed by the same nerve (CN(5) or the Trigeminal nerve). Other descriptions of pain may include: dull aches, background burning, sharp and throbbing in the general condyle area. Referral patterns for the muscles of mastication and other posterior spinal muscles which have implications on TMD may also incur migraines, forehead pain and patterns of ear pain. TMD patients will also note that stress, jaw clenching, teeth grinding (bruxism) and eating will aggravate and prolong the pain. While relaxing, local heating and analgesics will decrease this muscular pain.
The impact of TMD is greatly obstructive to sleep, eating and general quality of life. These symptoms may also amplify other comorbidities such as sinus pain, rheumatic disorders, magnify other musculo-oriented pain and increase risk of depression. Therefore it all TMD pain should be sought and rectified immediately for prophylactic management but also to return the patient to normal living standards.
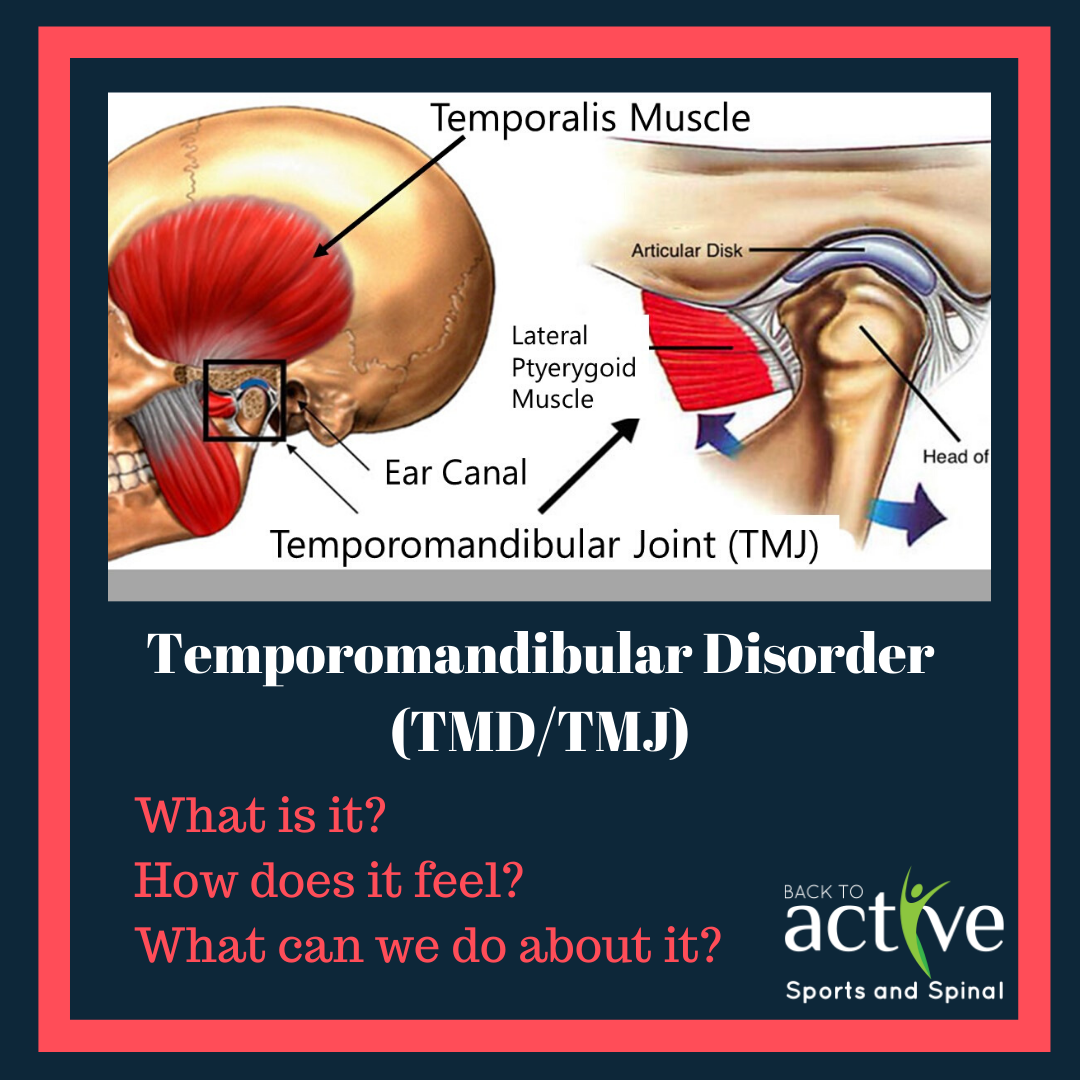
The main two groups of muscles that can contribute to TMD (as this is not a one dimensional injury – rather a trifecta of complications between muscle, jaw alignment and psychological) are:
- Muscles of mastication
- masseter,
- temporalis,
- lateral pterygoid,
- medial pterygoid.
- Cervical musculature
- Trapezius
- Cervical erector spinae
- Suprahyid muscles (digastrics, geniohyoid, stylohyoid and mylohyoid)
- Periscapular muscles
Locations responsible for producing referred pain to the different regions of the head.

What can we do?
With these muscle groups manual therapy in combination with exercises may show promising effects in decreasing localised pain in the area for patients with muscular (myogenous) TMD. What physiotherapy will do is assign passive and active stretching of muscles, and postural exercises. This is because exercises used to correct head and neck posture and active and passive oral exercises can be effective for reducing musculoskeletal pain and improving oromotor function. Manual therapy techniques such as mobilization of the cervical spine may also have a positive influence on orofacial pain followed by dry needling of cervical muscles to decrease acetylcholine activity in myofascial trigger points.
In short physiotherapy can contribute to decreasing muscular stiffness and referred pain, dentists can use occlusal splints to tend to malocclusion and psychologists may attend to any bruxism or teeth clenching secondary to anxiety and stress.
With the variable complaints that come with different presentations of TMD, it’s important to consider a tapered individual approach to every case. Clinicians can assess the needs of the patient to best guide them in an appropriate way.
Written by Joshua Shum Physiotherapist
