Hip bursitis / intertrochanteric bursitis
Have you taken a hiatus from running, come back and felt a niggle around your hip area? Or do you play soccer, rugby or oztag, adopted a new technique or training regime, then adopted a poorly localised hip pain? You’re not sure if it is your hip, yet it’s a sharp pain within your hip that only aggravates with certain movements. This may be something known as a trochanteric bursitis.
What is it?
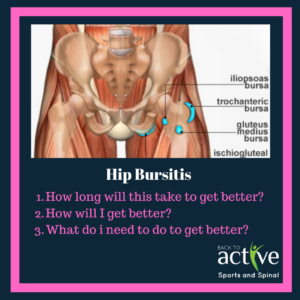
Most joints have a bubble known as a bursa. The bursa is a fluid-filled sac that facilitates in reducing friction between moving tissues of the body. It also assists as to cushion tensile force coming up into the hip. Bursitis is the inflammation of this sac.
There are two types of bursitis:
- Acute bursitis which is attributable to trauma or a massive overload.
- Chronic bursitis which is caused by overuse.
In either situation the inflamed bursa will cause lateral side hip pain due to a build up of fluid (effusion) within the sac.
One common cause for hip bursitis is due to glute medius weakness. This causes us to sway our hips which puts repetitive compression on that outer bursa every step that we take. Especially for runners, when running, if there is a biomechanical fault (trendelenburg gait) then this will need to be rectified.
Questions to answer:
- How long will this take to get better?
- Normally, symptoms of the bursa of the hip may be maintained within the first 1 or 2 weeks. However when attempting to get back to meaningful activities such as running or playing quick dynamic sports (soccer, netball, breakdancing, etc), it may take anywhere between 6 weeks to several months (or even up to a year). All bursitis generally respond very well to conservative treatment (exercises and decreasing repetitive stress), however some may resort to using cortisone to regulate the pain coming from the inflamed bursa.
- How will I get better/ what do I need to do specifically to get better?
- Evidence documents various treatments for any bursitis: immobilisation, cold packs/painkillers/ natural pain killers, antibiotics (if the bursa is bacterial), anabolic steroids (cortisone), surgical and conservative management; yet not all of these treatments will be suitable for your particular case. On that note the most important remedy for all bursitis is – identifying and deleting/minimising the irritant (maybe a fall or a repetitive stress such as dancing or jumping), appropriate rest then gradually increasing exercise load (specifically strengthening local muscle groups in the hip)
- Will I get better?
- Unless your bursitis is caused by an underlying gout or rheumatoid arthritic issue, mechanical bursitis is easily treated with conservative management. The biggest barrier to getting better is racing into an exercises or activity that is too overwhelming for your hip bursa. As the inflammation is a result of too much pressure on the bursa, we must make sure that exercise progression is appropriate and largely pain free.
- What exercises can I do to solve this problem?
- See below for a standard physio program for all hip bursitis
Signs and Symptoms
- Localised sharp lateral hip pain
- Referred pain either coming down the lateral side of the leg or into the groin region
- Painful when ascending stairs
- Painful on circular hip movement – i.e getting out of a car
- Unable to place pressure on affected side
Risk factors
- Women are greater than men
- Obesity
- Trauma
- Overuse
- Postural deficit
- Dysfunctional muscle/muscle control
- Osteoarthritis
- Poor running kinematics
- Right iliotibial band tightness
- Other inflammatory diseases (rheumatoid, gout)
- leg length discrepancy
Solution
Physiotherapy is strongly encouraged to identify the cause of the problem and implement strategies or modifications to certain activities. While managing bursitis, it is important to minimise all activities that would irritate the bursa. Conversely is best to identify what can be done and what exercises are appropriate to condition the hip. Physiotherapy will aid by improving hip strength, range of motion and rectifying any biomechanical faults that predisposed the patient to hip bursitis. The overarching goal is to bring out of pain but also set up prophylactic management strategies to avoid relapse.
Example program : by no means is this program a replacement for physiotherapy treatment, please read with discretion
For acute onset of hip bursitis its important to:
- Apply ice to the areas 2 – 3 times per night for 15 mins – anaesthetic effect.
- Identify all painful movements and avoid those specific painful movements if able – i.e running, abrupt turning, jumping
- Sport hiatus
To substitute sport or your previous exercise routine, the following exercises will be beneficial for you:
Introductory exercise – to be performed everyday instead of sport. All these exercises must be pain free before moving onto the next phase.
- Bridging with ball in between knees (performing a bridge with a foam roller in between your legs – squeeze your legs together) 3 x 10
- Glute foam rolling, piriformis stress, iliotibial band stretch and foam rolling. Each for 2 mins.
- Mini wall squats with ball squeeze 3 x 10
- Straight leg raise 3 x 10
- Ice twice daily over the hip 3x (15 mins at a time)
- Straight leg raise 3 x 10
Moderate exercises
- Hip tilts in standing 3 x 10
- Theraband clams 3 x 10
- Crab walks interval for 5 mins
- Straight line lunges 3 x 10
- Weighted hip thrusts on swiss ball 3 x 10
- Bosu ball squats 4 x 10
- Bosu ball jogging (dome side) 3 x 2 mins
- SIngle leg swiss ball bridge 4 x 8
Advanced exercises (balance + plyometric/sport specific)
- Weighted barbell squats + leg press + weighted deadlifts
- Single leg squat eccentric
- single leg deadlifts
- Bound jumps
- Skater jumps (+ variations of skater jump)
- Resistance band running drills
Sport specific exercises
- Sport specific activities + tentative/gradual return to sport
- Fixing biomechanical fault (i.e trendelenburg)
To facilitate a faster and safer return to sporting and activities of daily living physiotherapy is ideal for people suffering from hip bursitis. However, physiotherapy doesn’t just stop there, training and will seek to improve the patient better than how they were before their injury.
Article by Joshua Shum (Physiotherapist)
